In the Physician Fee Schedule final rule for calendar year 2026, CMS and its subsidiary agency, the Center for Medicare and Medicaid Innovation (CMMI), have finalized an alternative payment model for physician reimbursement: the Ambulatory Specialty Model (ASM). This mandatory model is designed for physicians treating heart failure and low back pain in ambulatory settings. These were selected because they are two of Medicare’s most prevalent and high-cost conditions.
The ASM exemplifies CMMI’s commitment to alternative payment models that promote value-based care and drive savings for CMS. If the model is successful, it could also provide a framework for CMMI to quickly scale the model to other common, high-cost, chronic conditions.
What Is the Purpose of the ASM?
The creation of the ASM reflects a broader initiative within the U.S. healthcare system to transition from traditional fee-for-service models toward value-based care. By adjusting Medicare Part B payments to specialists based on performance, the ASM aims to promote improvements in patient outcomes and decrease expenditures, while testing new ways to manage chronic diseases.
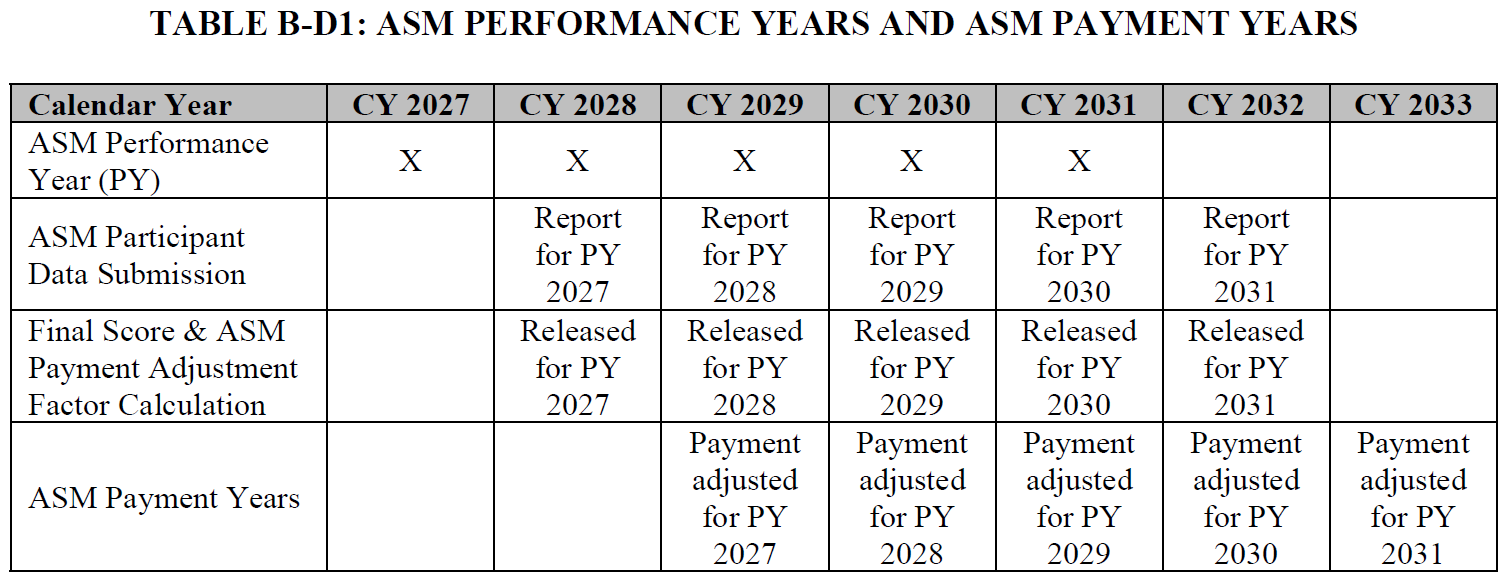
Performance in ASM will span five calendar years, from 2027 to 2031. Payment adjustments from outcomes during this period will take effect over five subsequent calendar years, from 2029 to 2033.
At its core, the ASM will assess whether incentivizing physicians through positive or negative payment adjustments based on a performance evaluation can effectively enhance quality and reduce costs. The model is based on the Merit-Based Incentive Payment System (MIPS) performance categories and uses the quality, cost, improvement activities, and promoting interoperability domains to determine performance.
Who Is Selected to Participate in the ASM?
The ASM differs from some previous alternative payment models in that participation is mandatory for physicians in selected core-based statistical areas (CBSAs) or metropolitan divisions who meet the established eligibility criteria. The CBSAs and metropolitan divisions were selected at random, with a 40% probability, from within each of the following stratified groups:
- CBSAs with low average episode spending & low episode volume
- CBSAs with low average episode spending & high episode volume
- CBSAs with high average episode spending & low episode volume
- CBSAs with high average episode spending & high episode volume
- CBSAs with very high episode volume
- Metropolitan divisions
This methodology is intended to promote a representative sample of diverse practice settings, cost levels, and patient demographics.
To qualify for ASM, physicians must have at least 20 attributed episodes of heart failure or low back pain during the measurement period, as calculated by MIPS Episode-Based Cost Measures (EBCMs). CMS has clarified that it will select physicians at the individual physician level, not as a practice group. Physicians who practice in multiple CBSAs or metropolitan divisions will be assigned to the area where they had the majority of their episodes. CMS will utilize 2025 data to confirm physician eligibility.
As of December 2025, CMS has released the list of selected geographic areas. A preliminary list of participating physicians within these geographic areas is expected to be announced by the end of July 2026.
Specialties included in the model for low back pain will be anesthesiology, pain management, interventional pain management, neurosurgery, orthopedic surgery, and physical medicine and rehabilitation. General cardiology is the only specialty included for heart failure.
How Will Physician Performance & Payment in the ASM Be Assessed?
The ASM will use a sophisticated payment adjustment system based on how the physician performs in four areas: quality, cost, improvement activities (IA), and promoting interoperability (PI).
Quality and cost each constitute 50% of the overall performance score. Physicians will be evaluated within condition-specific cohorts; thus, heart failure specialists will be compared exclusively with peers managing the same condition, as will those treating low back pain.
For the quality component, each cohort will be assigned a set of mandatory measures, such as the administration of beta-blocker therapy, ACE inhibitors/ARBs/ARNIs, blood pressure control, and functional status measurement for heart failure. Physicians will earn points based on their reported outcomes compared to decile-based benchmarks derived from ASM participant data in that episode cohort. Failure to report the required measure will result in a score of zero for that metric, lowering the possible payment amount for that physician.
The cost component will be evaluated based on a physician’s average risk-adjusted expenditures against cohort benchmarks, with a minimum threshold of 20 attributed episodes required for scoring. The lower the average cost a physician achieves compared to their peers, the more points they will earn, which will increase their payment.
The IA component will require physicians to attest to the completion of two distinct actions: establishing referral connections with primary care and ensuring the completion of health-related social needs screenings, as well as formalizing communication and collaboration protocols with primary care practitioners. Physicians who complete both activities will not lose any points from their final score, while those who fail to complete one or both will have points deducted.
The PI component will require participants to utilize certified electronic health record (EHR) technology and report on designated PI objectives and measures. Failure to fulfill the requirements in this area will decrease the final score and lower the total possible payment a physician can receive.
See the table below for an overview of how these four domains will factor into the final score:
| Category | Measure Type | Examples | Weighting |
|---|---|---|---|
| Quality | Condition-specific clinical & patient-reported outcomes |
| 50% |
| Cost | Episode-Based Cost Measures (EBCMs) | Per-episode Medicare spending compared to cohort median, risk-adjusted for the participant’s population | 50% |
| Improvement Activities |
|
| Up to −20 points |
| Promoting Interoperability |
|
| Up to −10 points |
The aggregate score based on these four domains will be translated into a payment adjustment factor via a logistic function. These positive, neutral, or negative adjustments will then be applied to Part B claims associated with heart failure or low back pain during the associated payment year.
Certain physicians, such as those managing more complex patient populations or practicing in smaller practices, may qualify for multiplier adjustments to their final scores, which will be applied before their payment adjustment is calculated.
What Is the Implementation Timeline for the ASM?
CMS anticipates announcing the initial group of mandatory geographic areas and physicians by the end of 2025 and utilizing 2025 data to finalize selections by July 2026.
Performance measurement for the ASM will begin in 2027 and conclude at the end of 2031. The corresponding payment adjustment year will be two years after each performance year, as outlined in the table below.
How Will the ASM Drive Savings for CMS?
The ASM model closely aligns with directives from the House Ways and Means Committee, as articulated in an April 28 letter to CMMI. This letter advocated for the development of value-based models that prioritize efficiency and cost savings. ASM is among the first new models announced after this directive with the goal to promote higher quality and lower-cost care, while exploring the impact of a new reimbursement model.
Unlike MIPS, which is budget-neutral, the ASM will drive savings for CMS. Under the ASM, CMS will retain a portion of the Part B reimbursement, starting at 1.35% of physician payments for relevant episodes in the first year and rising to 1.80% by the fifth year. The retained portion is anticipated to contribute materially to overall Medicare savings and is not included in the incentive pool that will be used to pay out bonuses or penalties. Using this approach, CMMI is in essence guaranteeing itself savings, which will likely allow the model to be expanded to other geographies and conditions.
In addition to direct savings, the model’s design encourages changes in chronic care management, enhanced care coordination, and adoption of interoperable health records, which should help lower the cost of chronic care management for the beneficiaries involved. CMS contends that this model will be successful in reducing unnecessary imaging and procedures for lower back pain and hospitalizations and emergency department visits for heart failure.
How Should Physicians Prepare for the ASM?
The ASM model is complex and represents a significant shift in Medicare Part B reimbursement, so physicians who may be required to participate should start preparing now. A good place to start is with a careful review of the eligibility criteria to understand whether your practice is likely to be included. CMS will utilize the MIPS EBCMs to attribute episodes to physicians, and understanding which cases will be attributed to you is vital.
Next, physicians should assess their current performance on the quality and cost measures the ASM will use. This includes reviewing your practice’s outcomes in the selected quality metrics and understanding your current episode-based costs. Understanding how quality and cost are measured and the variables you can adjust to improve performance will help position your practice to succeed within the model.
Physicians will also need to confirm that they will fulfill the requirements in the IA and PI components of the model, as these areas will affect the reimbursement penalty and may take time to implement. Because ASM scoring will be based on a combination of quality, cost, IA, and PI, practices should establish robust processes for data collection, reporting, and continuous quality improvement. Engaging clinical and administrative staff in education about ASM requirements and performance categories will be essential.
Finally, it is important to model the financial impact of ASM payment adjustments for both possible upside and downside so your organization can plan for revenue changes and identify opportunities to improve performance bonuses. Early preparation and proactive engagement can help physicians reduce uncertainty and create a road map for success.
How Forvis Mazars Can Help
Our value-based care professionals have extensive experience supporting providers in alternative payment models. We will continue to monitor CMS communications and the Federal Register and provide updates on the model as they become available. In the meantime, if you have questions or would like assistance preparing for the ASM, please reach out to our team today.
